Peripheral Artery Disease (PAD)
Peripheral artery disease (PAD), also known as Peripheral Vascular Disease (PVD), is a narrowing of the peripheral arteries serving the legs, stomach, arms and head. “Peripheral” in this case means away from the heart, in the outer regions of the body. PAD most commonly affects arteries in the legs.
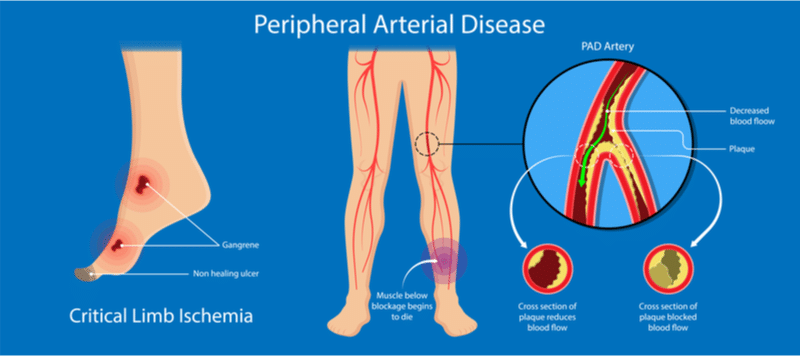
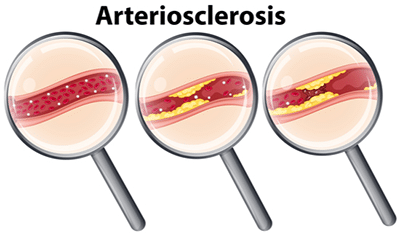
Both PAD and coronary artery disease (CAD) are caused by atherosclerosis which is a buildup of a fatty substance called Plaque.
How is PAD diagnosed?
PAD diagnosis begins with a physical examination and discussion about any symptoms you may be experiencing. We will check for weak pulses in the legs. Your physical examination may include the following:
- Ankle-brachial index (ABI): a painless exam that compares the blood pressure in your feet to the blood pressure in your arms to determine how well your blood is flowing. This inexpensive test takes only a few minutes and can be performed by your healthcare professional as part of a routine exam. Normally, the ankle pressure is at least 90 percent of the arm pressure, but with severe narrowing it may be less than 50 percent.
- Doppler and Ultrasound (Duplex) imaging: a non-invasive method that visualizes the artery with sound waves and measures the blood flow in an artery to indicate the presence of a blockage.
- Computed Tomographic Angiography (CT): a non-invasive test that can show the arteries in your abdomen, pelvis and legs. This test is particularly useful in patients with pacemakers or stents.
If these tests reveal possible abnormal findings then your doctor may recommend one of these other tests.
- Magnetic Resonance Angiography (MRA): a non-invasive test that gives information similar to that of a CT without using X-rays.
- Peripheral Angiogram: During an angiogram, also called an arteriogram, a contrast agent is injected into the artery and X-rays are taken to show blood flow through arteries in the legs and to pinpoint any blockages that may be present. Learn more about peripheral angiogram.
Treatment for Peripheral Artery Disease at San Tan Cardiovascular Center
Treatment for peripheral artery disease (PAD) focuses on reducing symptoms and preventing further progression of the disease. In most cases, lifestyle changes, exercise and claudication medications are enough to slow the progression or even reverse the symptoms of PAD.
Physical Activity
An often effective treatment for PAD symptoms is regular physical activity. Your doctor may recommend a program of supervised exercise training for you, also known as cardiac rehabilitation.
You may have to begin slowly, but simple walking regimens, leg exercises and treadmill exercise programs can ease symptoms. Exercise for intermittent claudication – poor circulation in leg arteries due to buildup of plaque – takes into account the fact that walking causes pain. The program consists of alternating activity and rest in intervals to build up the amount of time you can walk before the pain sets in.
It’s best if this exercise program is undertaken in a rehabilitation center on a treadmill and monitored. If it isn’t possible to go to a rehabilitation center, your healthcare professional may recommend a structured community or home-based program that’s best suited to your situation.
Learn more about our Cardiac Rehab Services.
Diet
Many PAD patients have elevated cholesterol levels. A diet low in saturated and trans fat can help lower blood cholesterol levels, but cholesterol-lowering medication may be necessary to maintain the proper cholesterol levels.
The Cardiac Rehab Center at San Tan Cardiovascular offers many useful brochures to help you stick to a healthy diet.
Smoking Cessation
Tobacco smoke is a major risk factor for PAD and your risk for heart attack and stroke. By quitting smoking it will help to slow the progression of PAD and other heart-related diseases.
Learn how you can kick the habit – Quit Smoking / Tobacco / Vaping.
Medication
You may be prescribed high blood pressure medications and/or cholesterol-lowering medications. You may also be prescribed medication to help prevent blood clots.
It is important to make sure that you take the medication as recommended by your healthcare professional. Not following directions increases your risk for PAD, as well as heart attack and stroke.
Managing Diabetes
Working with a coordinated healthcare team and making the lifestyle changes necessary to best manage diabetes may help reduce limb-related complications.
Medical Procedures
Peripheral Angiogram
For a minority of patients, the above recommendations and treatments aren’t enough, and minimally invasive treatment or surgery may be needed.
Angioplasty or stent placement (as is done in the heart for coronary artery disease (CAD)) are nonsurgical and are performed by inserting a small catheter to reach the blocked artery. A tiny balloon is inflated inside the artery to open the blockage. A stent — a tiny wire mesh cylinder — may also be implanted at this time to help hold the artery open. Atherectomy is a procedure to remove plaque from the artery wall to help the balloon and stent stay open.
San Tan Cardiovascular Center has a state-of-the art Angiography Cath Lab Suite on location that offers superior treatment to our patients. Our Cath Lab team has over 70 years combined experience between the staff. We offer hospital quality care and surgical treatment in a comfortable outpatient setting.
Peripheral Artery Bypass Graft Surgery
If the blockage in your leg artery is completely blocked or the area blocked is in a location the physician feels might be unsafe for angioplasty then bypass surgery may be necessary. Using a special plastic “graft” material or a vein from another part of the body can help “bypass” and reroute blood around the blocked artery.
Your physician will discuss your options and help choose the best procedure for your situation.
As stated earlier, PAD often goes undiagnosed. Untreated PAD can be dangerous because it can lead to painful symptoms or loss of a leg, and patients with PAD have an increased risk of coronary artery disease, stroke and heart attack. Because people with PAD have this increased risk for heart attack and stroke, the American Heart Association encourages people at risk to discuss PAD with their healthcare professional to ensure early diagnosis and treatment.
How do I get started?
Contact San Tan Cardiovascular Center today to make an appointment with one of our healthcare providers.
At this appointment:
- we will review your medical history, discuss your symptoms and perform a non-invasive, diagnostic test to further determine your medical condition,
- any pertinent testing that needs to be done beforehand will also be ordered at this time.
Our billing department will then contact your health insurance company to obtain prior authorization. Upon receiving insurance authorization, the treatment will be scheduled.
Peripheral Artery Disease FAQs
Q: What are the symptoms of Peripheral Artery Disease (PAD)?
A: The most common symptoms of PAD involving the lower extremities are:
- Leg cramping
- Pain, typically when you walk
- Tiredness in the leg or hip muscles while walking or climbing stairs
- Numbness of the legs or feet
- Buttock pain
- Burning or tingling in the feet
- Sores or breaks in the skin of the legs and feet
- Loss of hair on the feet or toes
- Changes in skin color (reddish, bluish, or pale discoloration)
- Decrease in skin temperature
- Impotence (inability to get or maintain an erection)
Be aware that:
- Many people mistake the symptoms of PAD for something else.
- PAD often goes undiagnosed by healthcare professionals.
- People with peripheral arterial disease have a higher risk of coronary artery disease, heart attack or stroke.
- Left untreated, PAD can lead to feet ulcers, gangrene and amputation.
It is Important to note that, in many instances, diabetic patients are too quickly misdiagnosed with having diabetic neuropathy instead of investigating further and ruling out peripheral artery disease. These patients might be prescribed unnecessary medications for the neuropathy pain while the underlying cause is not being treated.
Q: What are the risk factors for Peripheral Artery Disease?
- Age over 50 years old
- Smoking
- Diabetes
- Family history of heart or vascular disease
- High blood pressure (also called hypertension)
- High levels of cholesterol and triglycerides in your blood
- Lack of exercise or physical activity
- Obesity (overweight)
- Stress